Sex, Drugs, and Serotonin

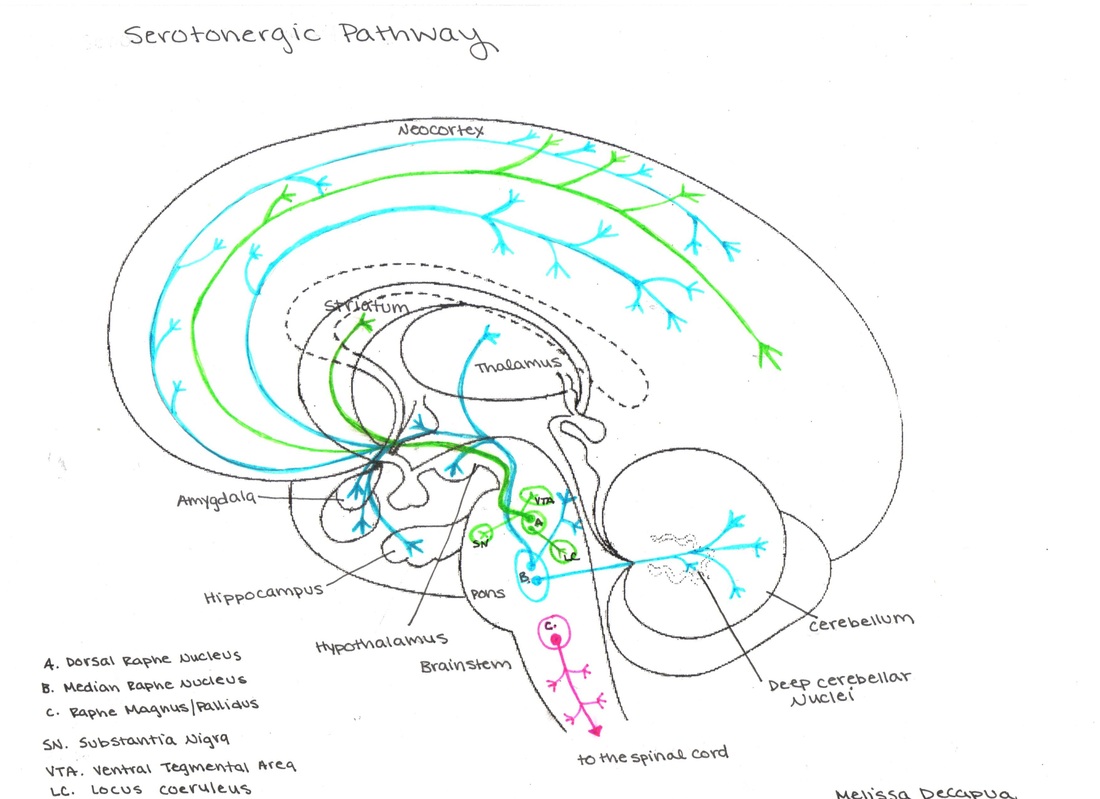
Serotonin, a monoamine neurotransmitter, is closely associated with modern psychiatry, and is a common target in psychopharmacology. Generally, this neurotransmitter effects mood, appetite, and sleep. Serotonin is synthesized from the amino acid tryptophan in the cell body of specific neurons, which are primarily located in the raphe nuclei in the brainstem: pertinently, the dorsal raphe nucleus (colored green in the diagram below), median raphe nucleus (blue), and raphe magnus/pallidus (pink).
Falling asleep already? Try this for some blog-reading background music. (I think I just gave away my Indiana roots).
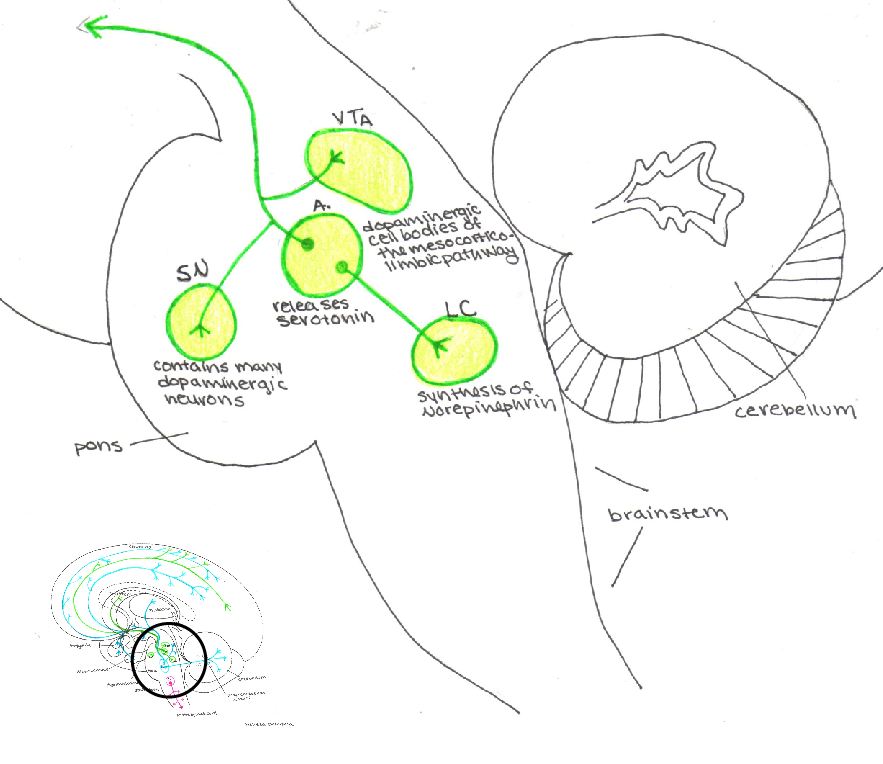
The dorsal raphe nucleus innervates the dopaminergic neurons in the substantia nigra (SN) and ventral tegmental area (VTA) and thus influences the output of dopamine. This nucleus also receives input from the locus coeruleous via norepinephrine. It then projects through the median forebrain bundle to the striatum and spreads throughout the entire cortex (Pliszka 2003).
The median raphe nucleus also projects through the median forebrain bundle to the amygdala, hippocampus, and the suprachiasmatic nuclei of the hypothalamus, thereby influencing the emotional responses, memory and circadian rhythm. Furthermore, it projects to the superior colliculi, cerebellum, and also out through the entire cortex (Pliszka 2003).
The raphe magnus pallidus projects caudally and terminates in the dorsal horn of the spinal grey matter where it regulates pain sensations. These projections also synapse on motor neurons to determine the strength of reflexes and innervate the intermediolateral cell column, thus playing a role in the output of the sympathetic nervous system (Pliszka 2003).
Let’s Get Things Straight
When All’s Well
When the serotonergic brain pathway is functioning properly it regulates many aspects of mood, behavior, and physiological responses including affect and anxiety. This system modulates these bodily functions through its dynamic relationship with the other two monoamines: norepinephrine (NE) and dopamine (DA). While NE tells the body what to pay attention to, DA facilitates action (Pliszka 2003). The serotonin system functions to balance these two behaviors.
Generally, serotonin has an inhibitory effect on NE, thus determining when a person has paid enough attention to stimuli. Serotonin then “hands off” this information to the dopamine system, which in turn reacts to the stimuli (Pliszka 2003). The dorsal raphe nucleus plays the central role in this process by receiving input directly from the locus coeruleous and projecting to the SN and VTA.
Overall, serotonin facilitates the formation of adaptive behavior by balancing these other two systems (Pliszka 2003). In conclusion, when functioning optimally, the serotonin system governs a variety of physiologic tasks including feeding, sleeping, pain sensations, reflexes, and mood.
When All’s Not So Well
There are various clinical manifestations of a perturbed serotonergic system. First, excess serotonergic activity results in a dangerous adverse reaction called Serotonin Syndrome, or serotonin toxicity. A patient affected by too much serotonin would appear tachycardic, diaphoretic, myoclonic, hypertensive, agitated, mydriatic, hyperreflexive, and hypervigilant. In severe cases, without intervention, Serotonin Syndrome can lead to cardiogenic shock and death (Fortinash 2008).
Another example of a perturbed serotonergic system is called Antidepressant Discontinuation Syndrome, which occurs with the withdrawal of antidepressant medications. In contrast to Serotonin Syndrome, this reaction results from a deficiency of serotonin and presents with flu-like symptoms, insomnia, nausea, gait imbalance, hyperarousal, and sensory disturbances (Warner 2006).
Furthermore, some psychedelic drugs effect the serotonergic pathway and cause it to function abnormally. Lysergic acid diethylamide (LSD), a 5HT2A/2C receptor agonist, causes changes in perceptions such as the illusions of moving walls, amplification of colors, and transitory dissociation (Kring 2007). MDMA, or ecstasy, causes a burst of serotonin (along with other monoamines) in the central nervous system leading to euphoria, decreased anxiety, and sense of closeness with others (Kring 2007). Finally, serotonergic pathway dysfunction has been implicated in various psychiatric disorders and will be discussed in the next section.
Psychiatric Disorders & Serotonin
Demographic, Epidemiological & Lifespan Considerations
Vigorously researched, serotonin has been shown to play a role in depression, anxiety, eating disorders, obesity, aggressive behavior, sexual dysfunction, migraines, and chronic pain (Pliszka 2003). For many psychiatric disorders, their successful treatment with medications which increase the availability of serotonin at the synapse provide some evidence of the involvement of this neurochemical.
Recently, for example, neuroimaging research of patients with psychiatric illnesses revealed abnormalities in the number of serotonin receptors in the prefrontal cortex, amygdala, hypothalamus, nucleus accumbens, and hippocampus all of which have some effect on mood, pleasure, appetite, sleep, concentration, and suicidal ideation (Kraly 2009).
Two dysfunctions of the serotonin pathway discussed above were Serotonin Syndrome (SS) and Antidepressant Discontinuation Syndrome (ADS). From an epidemiological perspective, the incidence of SS is unknown, and there is no current data suggesting gender or demographic related vulnerabilities; however, lack of education of both the provider and patient can contribute to complications (Stern 2008).
Given its overlap with Neuroleptic Malignant Syndrome, SS can be misdiagnosed or underreported. For patients who overdose on Selective Serotonin Reuptake Inhibitors (SSRIs), about 14%-16% develop SS (Stern 2008). On the other hand, those at most risk for developing ADS are women who find out they are pregnant and patients who cannot afford their medication (Warner 2006). Moreover, without proper education, some patients may choose to discontinue their medication once they begin to feel better (Warner 2006).
As the body ages, so does the brain. Pertinent age related changes include a significant decline in monoamine synthesis and an increase in monoamine oxidase (Birren 1980). According to Birren and Sloane, cerebral blood flow and oxygen consumption remain steady through the lifespan, but brain glucose utilization drastically declines (1980).
If you want some more light reading on serotonin, be sure to check out these awesome books.
Share on Facebook Share on Twitter Share on Pinterest
0 Comments on "Sex, Drugs, and Serotonin"